It’s cervical awareness month, so let’s talk about HPV – the most common STI infecting about 80% of people who are sexually active.
Despite it being so common, many of us were not taught much about it. We know about the recommendations for regular cervical screening, but without information about what HPV is, many are left unsure why they are getting these ‘uncomfortable’ tests done to begin with. After many conversations, I’ve realized how many people haven’t had screening done since 2019. So let’s talk about it!
What is HPV?
Human Papillomavirus, or HPV, is a diverse family of viruses with over 200 different strains.
These strains are categorized into low-risk and high-risk. Low-risk strains might cause warts, while high-risk strains are associated with various cancers, including cervical cancer. Many people infected with HPV do not develop any symptoms at all, making it difficult to detect and diagnose without screening. This is why screening is essential.
How do I test for HPV?
For a long time, pap tests have been the method of choice when it came to cervical screening. Canada, and many other countries, are shifting to HPV tests aiming for a more accurate and reliable detection of high-risk HPV strains. Remember, having a high-risk strain or abnormal test results do not indicate cancer. Many people can actually clear the infection on their own; we will talk more about the results and clearing HPV in the next blog.
What is the difference between pap tests and HPV tests?
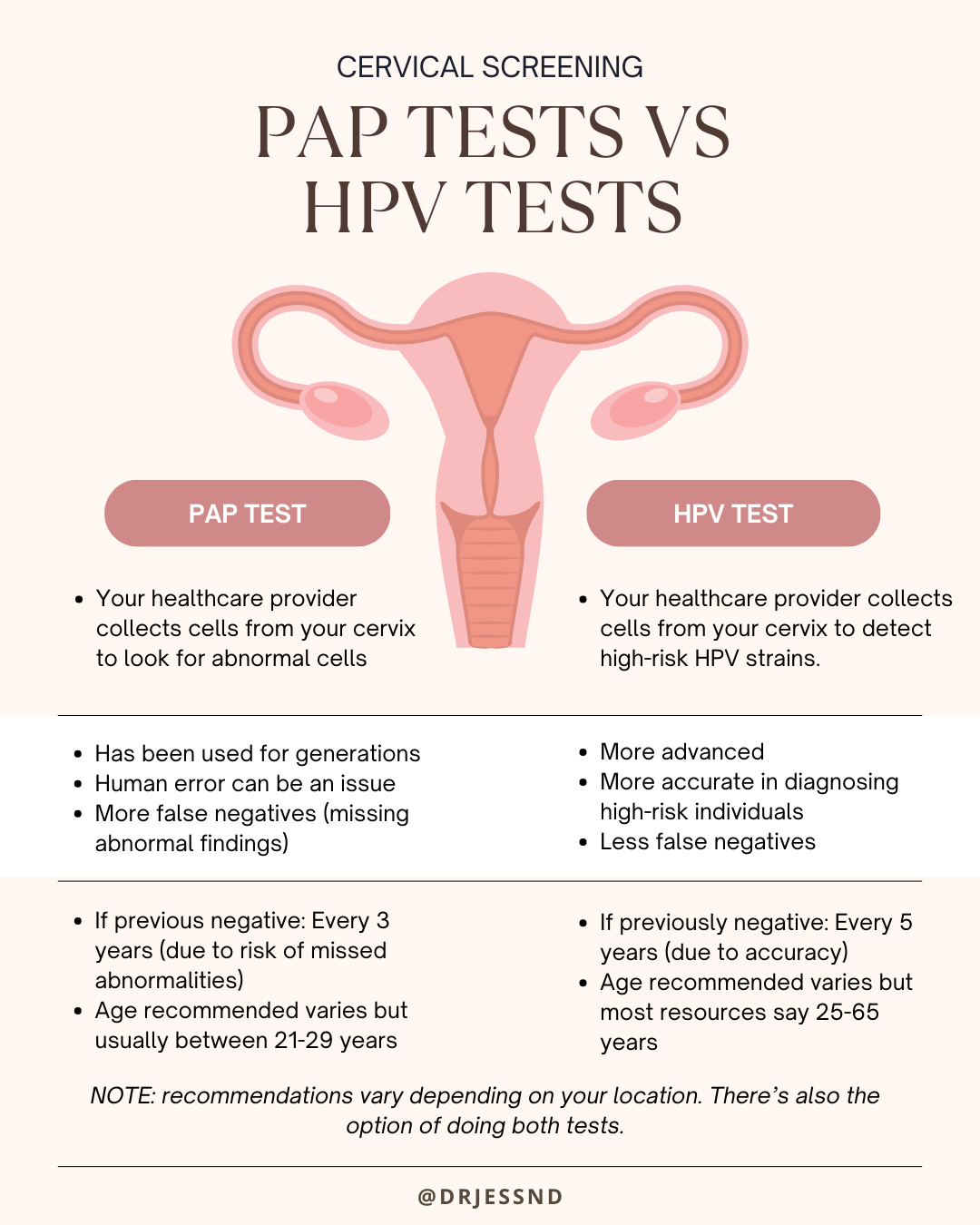
There’s been a lot of pushback in different countries with the shift towards HPV testing: some are worried about the lower frequency of testing, others are wondering if it’s a cost-saving change, and some just like to stick to what they’re used to. Trust me, I get these concerns.
After looking into recommendations across different countries and organizations, here are my thoughts:
- Pap tests seem to give more false negatives than HPV testing. This means that paps might miss some abnormalities.
- Some suggest waiting for HPV testing until after the age of 25, using pap tests from 21-25, to prevent an excess of false positives at this age due to the prevalence of HPV. False positives lead to more invasive investigations that are unnecessary and can have complications.
- With cervical cancer being diagnosed mainly between ages 35-45, HPV testing starting at 25, allows for ample opportunity to detect high-risk HPV strains
- The switch from every 3 years to every 5 is mainly due to the higher likelihood that the pap test will miss abnormalities, requiring more frequent testing. Based on the current research, the probability of finding a precancerous lesion 10 years after a single negative HPV test is less than 1%.
Understanding what HPV is, why screening matters, and the recommendations for regular check-ups equip you to take charge of your reproductive health.
Remember to follow the recommended guidelines for cervical screening, but also be aware that individual circumstances may require a different screening schedule. Certain locations, including Ontario, have not yet rolled out the switch. Talk to your healthcare provider to determine the appropriate frequency and timing based on your personal risk factors.


Next Steps
If you know you’re due for a test or you can’t remember the last time you had one, talk to your doctor. I also offer Empowered Paps to Ontario residents at the clinic: PAP testing that is adapted to your pace, ease and comfort. This can be especially helpful for those with negative previous experiences, vaginismus, pain with insertion, or other anxieties around the test itself. If you want to learn more, book a free discovery call with me here.
Be well,
Dr. Jess

